627:
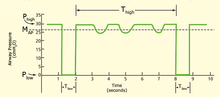
controlled modes, it does not rely on a passive expiration created by collapse of the thoracic wall and elastic recoil of the lungs. A high resistant breathing circuit inhibits a passive expiration and therewith allows to fully control and stabilize the expiration flow. FCV creates an inspiration by generating a stable flow from a set End-expiratory pressure (EEP) to a set Peak pressure. Then a stable expiratory flow is created by suctioning. This expiratory flow rate is preferably similar to the inspiratory flow, aiming for an I:E ratio of 1:1.0, to minimize energy dissipation in the lungs. FCV® is a more efficient ventilation as compared to conventional modes, allows ventilation through even small lumens (~2 – 10 mm ID) and results in less applied mechanical power. FCV was invented by
Professor Dr. med. Dietmar Enk.
211:
inspiratory flow or pressure and rise time (set-point targeting), tidal volume (dual targeting) and constant of proportionality between inspiratory pressure and patient effort (servo targeting). Examples of between-breath targets and targeting schemes include average tidal volume (for adaptive targeting), percent minute ventilation (for optimal targeting) and combined PCO2, volume, and frequency values describing a "zone of comfort" (for intelligent targeting, e.g., SmartCarePS or
IntelliVent-ASV). The targeting scheme (or combination of targeting schemes) is what distinguishes one ventilatory pattern from another. There are 7 basic targeting schemes that comprise the wide variety seen in different modes of ventilation:
359:
25:
193:
signals representing the patient determined components of the equation of motion, (ie, elastance or resistance and including effects due to inspiratory effort). Flow cycling is a form of patient cycling because the rate of flow decay to the cycle threshold is determined by patient mechanics. Machine cycling means ending inspiratory time independent of signals representing the patient determined components of the equation of motion.
652:," a tank in which the patient lays, with only their head exposed to ambient air, while air pressure on the remainder of their body, inside the tank, is varied by pumping, to stimulate chest and lung expansion and contraction. Though not in wide use today, NPVs were the principal forms of hospital and long-term mechanical ventilation in the first half of the 20th century, and remain in limited use today.
769:
419:) differs by ventilator brand and model, but, in general, there is a window of monitored time, and a smaller window checked against the larger window (i.e., in the Dräger Evita® line of mechanical ventilators there is a moving 20-second window, and every 7 seconds the current tidal volume and rate are measured) to decide whether a mechanical breath is needed to maintain the minute ventilation.
383:, a very similar mode, biphasic positive airway pressure (BIPAP), was introduced in Europe. The term APRV has also been used in American journals where, from the ventilation characteristics, BIPAP would have been perfectly good terminology. But BiPAP(tm) is a trademark for a noninvasive ventilation mode in a specific ventilator (Respironics Inc.).
666:
the ventilator are automatically adjusted and optimized to mimic natural breathing, stimulate spontaneous breathing, and reduce weaning time. In the ASV mode, every breath is synchronized with patient effort if such an effort exists, and otherwise, full mechanical ventilation is provided to the patient.
747:
In total liquid ventilation (TLV), the entire lung is filled with an oxygenated PFC liquid, and a liquid tidal volume of PFC is actively pumped into and out of the lungs. A specialized apparatus is required to deliver and remove the relatively dense, viscous PFC tidal volumes, and to extracorporeally
644:
Negative-pressure ventilation stimulates (or forces) breathing by periodic application of partial vacuum (air pressure reduced below ambient pressure), applied externally to the patient's torso—specifically, chest and abdomen—to assist (or force) the chest to expand, expanding the lungs, resulting in
606:
In
Pressure Support, the set inspiratory pressure support level is kept constant and there is a decelerating flow. The patient triggers all breaths. If there is a change in the mechanical properties of the lung/thorax and patient effort, the delivered tidal volume will be affected. The user must then
274:
Step 1: Identify the primary breath control variable. If inspiration starts with a preset inspiratory pressure, or if pressure is proportional to inspiratory effort, then the control variable is pressure. If inspiration starts with a preset tidal volume and inspiratory flow, then the control variable
198:
Breaths are classified as spontaneous or mandatory based on both the trigger and cycle events. A spontaneous breath is a breath for which the patient both triggers and cycles the breath. A spontaneous breath may occur during a mandatory breath (e.g. Airway
Pressure Release Ventilation). A spontaneous
170:
In this equation, pressure, volume, and flow are all continuous functions of time. Pressure is actually a pressure difference across the system (e.g., transrespiratory pressure defined as pressure at the airway opening minus pressure on the body surface). Elastance (defined as the change in pressure
163:
A ventilator assists breathing using either pressure control or volume control based on the equation of motion for the respiratory system. Providing assistance means doing work on the patient, which is accomplished by controlling either pressure or volume. A simple mathematical model describing this
159:
A breath is assisted if the ventilator does work on the patient. An assisted breath is one for which the ventilator does some portion of the work of breathing. For constant flow inflation, work is defined as inspiratory pressure multiplied by tidal volume. Therefore, an assisted breath is identified
665:
Adaptive
Support Ventilation (ASV) is the only commercially available mode that uses optimal targeting. This ventilation mode was invented and subsequently patented in 1991 by Dr. Fleur Tehrani In this positive pressure mode of ventilation, the frequency and tidal volume of breaths of a patient on
529:
refers to the ventilator's forced expiratory system. In a HFV-A scenario, the ventilator uses pressure to apply an inspiratory breath and then applies an opposite pressure to force an expiratory breath. In high-frequency oscillatory ventilation (sometimes abbreviated HFOV) the oscillation bellows
155:
A breath is one cycle of positive flow (inspiration) and negative flow (expiration) defined in terms of the flow-time curve. Inspiratory time is defined as the period from the start of positive flow to the start of negative flow. Expiratory time is defined as the period from the start of expiratory
386:
Other manufacturers have followed with their own brand names (BILEVEL, DUOPAP, BIVENT). Although similar in modality, these terms describe how a mode is intended to inflate the lung, rather than defining the characteristics of synchronization or the way spontaneous breathing efforts are supported.
202:
There are 3 breath sequences: Continuous mandatory ventilation (CMV), Intermittent
Mandatory Ventilation (IMV), and Continuous Spontaneous Ventilation (CSV). A breath sequence is a particular pattern of spontaneous and/or mandatory breaths. The 3 possible breath sequences are: continuous mandatory
192:
Patient triggering means starting inspiration based on a patient signal independent of a machine trigger signal. Machine triggering means starting inspiratory flow based on a signal from the ventilator, independent of a patient trigger signal. Patient cycling means ending inspiratory time based on
132:
familiarity and institutional preferences, since there is a paucity of evidence indicating that the mode affects clinical outcome. The most frequently used forms of volume-limited mechanical ventilation are intermittent mandatory ventilation (IMV) and continuous mandatory ventilation (CMV). There
1478:
Yañez, LJ; Yunge, M; Emilfork, M; Lapadula, M; Alcántara, A; Fernández, C; Lozano, J; Contreras, M; Conto, L; Arevalo, C; Gayan, A; Hernández, F; Pedraza, M; Feddersen, M; Bejares, M; Morales, M; Mallea, F; Glasinovic, M; Cavada, G (September 2008). "A prospective, randomized, controlled trial of
437:
For example, if a target tidal volume of 500 mL is set but the ventilator delivers 600 mL, the next breath will be delivered with a lower inspiratory pressure to achieve a lower tidal volume. Though PRVC is regarded as a hybrid mode because of its tidal-volume (VC) settings and pressure-limiting
542:
refers to the ventilator's non-forced expiratory system. In a HFV-P scenario, the ventilator uses pressure to apply an inspiratory breath and then returns to atmospheric pressure to allow for a passive expiration. This is seen in High-Frequency Jet
Ventilation, sometimes abbreviated HFJV. Also
210:
Within each ventilatory pattern there are several variations that can be distinguished by their targeting scheme(s). A targeting scheme is a description of how the ventilator achieves preset targets. A target is a predetermined goal of ventilator output. Examples of within-breath targets include
551:
Volume guarantee an additional parameter available in many types of ventilators that allows the ventilator to change its inspiratory pressure setting to achieve a minimum tidal volume. This is utilized most often in neonatal patients who need a pressure controlled mode with a consideration for
483:(NIV). First used in 1988 by Professor Benzer in Austria, it delivers a preset inspiratory positive airway pressure (IPAP) and expiratory positive airway pressure (EPAP). BPAP can be described as a Continuous Positive Airway Pressure system with a time-cycle change of the applied CPAP level.
1729:
Sebrechts T, Morrison SG, Schepens T, Saldien V. Flow-controlled ventilation with the Evone ventilator and
Tritube versus volume-controlled ventilation: a clinical cross-over pilot study describing oxygenation, ventilation and haemodynamic variables. Eur J Anaesthesiol 2021; 38: 209-211. doi:
626:
Flow-controlled ventilation (FCV) is an entirely dynamic ventilation mode, without pauses, with continuous and stable gas flows during both inspiration and expiration, aiming for linear changes in both volume and pressure. FCV is an invasive ventilation mode but, unlike Volume- and pressure
264:
The "primary breath" is either the only breath there is (mandatory for CMV and spontaneous for CSV) or it is the mandatory breath in IMV. The targeting schemes can be represented by single, lower case letters: set-point = s, dual = d, servo = r, bio-variable = b, adaptive = a, optimal = o,
756:
In partial liquid ventilation (PLV), the lungs are slowly filled with a volume of PFC equivalent or close to the FRC during gas ventilation. The PFC within the lungs is oxygenated and carbon dioxide is removed by means of gas breaths cycling in the lungs by a conventional gas ventilator.
244:
A mode of ventilation is classified according to its control variable, breath sequence, and targeting scheme(s). The preceding 9 maxims create a theoretical foundation for a taxonomy of mechanical ventilation. The taxonomy is based on these theoretical constructs and has 4 hierarchical
177:
Pressure control (PC) means that inspiratory pressure is preset as either a constant value or it is proportional to the patient's inspiratory effort. In other words, the left-hand side of the equation of motion remains constant while volume and flow change with changes in elastance and
206:
There are 5 basic ventilatory patterns: VC-CMV, VC-IMV, PC-CMV, PC-IMV, and PC-CSV. The combination VC-CSV is not possible because volume control implies machine cycling and machine cycling makes every breath mandatory, not spontaneous. A sixth pattern, TC-IMV is possible but
160:
as a breath for which airway pressure (displayed on the ventilator) rises above baseline during inspiration. An unassisted breath is one for which the ventilator simply provides the inspiratory flow demanded by the patient and pressure stays constant throughout the breath.
349:
A basic distinction in mechanical ventilation is whether each breath is initiated by the patient (assist mode) or by the machine (control mode). Dynamic hybrids of the two (assist-control modes) are also possible, and control mode without assist is now mostly obsolete.
199:
breath may be assisted or unassisted. A mandatory breath is a breath for which the machine triggers and/or cycles the breath. A mandatory breath can occur during a spontaneous breath (e.g., High
Frequency Jet Ventilation). A mandatory breath is, by definition, assisted.
188:
Trigger and cycle events can be initiated by the patient or the machine. Inspiration can be patient triggered or patient cycled by a signal representing inspiratory effort. Inspiration may also be machine triggered or machine cycled by preset ventilator thresholds.
1739:
Schmidt J, Wenzel C, Mahn M, et al. Improved lung recruitment and oxygenation during mandatory ventilation with a new expiratory ventilation assistance device: A controlled interventional trial in healthy pigs. Eur J Anaesthesiol 2018; 35: 736-744. doi: 10.1097/
824:
Esteban A, Anzueto A, Alía I, Gordo F, Apezteguía C, Pálizas F, Cide D, Goldwaser R, Soto L, Bugedo G, Rodrigo C, Pimentel J, Raimondi G, Tobin MJ (2000). "How is mechanical ventilation employed in the intensive care unit? An international utilization review".
341:). Invasive has to do with the insertion of medical devices or tubes internal to the patient, while non-invasive is completely external to the patient, as for example in using a tightly fitting mask or other device that covers the patient's nose and mouth.
203:
ventilation, (CMV, spontaneous breaths are not allowed between mandatory breaths), intermittent mandatory ventilation (IMV, spontaneous breaths may occur between mandatory breaths), and continuous spontaneous ventilation (CSV, all breaths are spontaneous).
721:
liquid rather than an oxygen-containing gas mixture. The use of perfluorochemicals, rather than nitrogen, as the inert carrier of oxygen and carbon dioxide offers a number of theoretical advantages for the treatment of acute lung injury, including:
137:
over the years, but more recently it has become standardized by many respirology and pulmonology groups. Writing a mode is most proper in all capital letters with a dash between the control variable and the strategy (i.e. PC-IMV, or VC-MMV etc.).
543:
categorized under High
Frequency Ventilation is High Frequency Percussive Ventilation, sometimes abbreviated HFPV. With HFPV it utilizes an open circuit to deliver its subtidal volumes by way of the patient interface known as the Phasitron.
468:(APAP) is a form of CPAP that automatically tunes the amount of pressure delivered to the patient to the minimum required to maintain an unobstructed airway on a breath-by-breath basis by measuring the resistance in the patient's breathing.
430:
Pressure-regulated volume control is an Assist Controlled Ventilation (ACV) based mode. Pressure-regulated volume control utilizes pressure-limited, volume-targeted, time-cycled breaths that can be either ventilator- or patient-initiated.
406:
Mandatory minute ventilation (MMV) allows spontaneous breathing with automatic adjustments of mandatory ventilation to the meet the patient's preset minimum minute volume requirement. If the patient maintains the minute volume settings for
414:
If the patient's minute volume is insufficient, mandatory delivery of the preset tidal volume will occur until the minute volume is achieved. The method for monitoring whether or not the patient is meeting the required minute ventilation
376:) is shortened to usually less than one second to maintain alveoli inflation. In the basic sense, this is a continuous pressure with a brief release. APRV currently the most efficient conventional mode for lung protective ventilation.
1749:
Schmidt J, Wenzel C, Spassov S, et al. Flow-controlled ventilation attenuates lung injury in a porcine model of acute respiratory distress syndrome: a preclinical randomized controlled study. Crit Care Med 2020; 48: e241-e248. doi:
1631:
Spieth PM, Carvalho AR, Güldner A, et al. (April 2011). "Pressure support improves oxygenation and lung protection compared to pressure-controlled ventilation and is further improved by random variation of pressure support".
1719:
Weber J, Schmidt J, Straka L, Wirth S, Schumann S. Flow-controlled ventilation improves gas exchange in lung-healthy patients – a randomized interventional cross-over study. Acta Anaesthesiol Scand 2020; 64: 481-488. doi:
1700:
Barnes T, van Asseldonk D, Enk D. Minimisation of dissipated energy in the airways during mechanical ventilation by using constant inspiratory and expiratory flows - flow-controlled ventilation (FCV). Med Hypotheses 2018;
171:
divided by the associated change in volume; the reciprocal of compliance) and resistance (defined as a change in pressure divided by the associated change in flow) are parameters assumed to remain constant during a breath.
1787:
Spraider, P. et al. Individualisedflow-controlled ventilation versus pressure-controlled ventilation in a porcine model of thoracic surgery requiring one-lung ventilation: A laboratory study. EurJ Anaesthesiol39, 885–894
1759:
Spraider, P, Martini J, Abram J, et al. Individualized flow-controlled ventilation compared to best clinical practice pressure-controlled ventilation: a prospective randomized porcine study. Crit Care 2020: 24: 662. doi:
1845:, "Early Positive and Alternate Pressure Machines" in "An Anesthesiologist's Perspective on the History of Basic Airway Management: The 'Progressive' Era, 1904 to 1960," submitted May 27, 2017, published February 2018,
1797:
Grassetto, A. et al. Flow-controlled ventilation may reduce mechanical power and increase ventilatory efficiency in severe coronavirus disease-19 acute respiratory distress syndrome. Pulmonology S2531-0437(22)00126-X
1769:
Schmidt J, Günther F, Weber J, et al. Glottic visibility for laryngeal surgery: tritube vs. microlaryngeal tube: a randomised controlled trial. Eur J Anaesthesiol 2019; 36: 963-971. doi: 10.1097/EJA. 0000000000001110.
224:
Optimal: A targeting scheme that automatically adjusts the targets of the ventilatory pattern to either minimize or maximize some overall performance characteristic (eg, minimize the work rate done by the ventilatory
174:
Volume control (VC) means that both volume and flow are preset prior to inspiration. In other words, the right hand side of the equation of motion remains constant while pressure changes with changes in elastance and
304:
The operator sets all the parameters of the volume and flow waveforms so the targeting scheme is set-point. Thus, the mode is classified as volume control continuous mandatory ventilation with set-point targeting
1778:
Meulemans J, Jans A, Vermeulen K, et al. Evone® flow-controlled ventilation during upper airway surgery: a clinical feasibility study and safety assessment. Front Surg 2020; 7: 6. doi: 10.3389/fsurg. 2020.00006.
317:
The operator sets the tidal volume but not the inspiratory flow. Because setting volume alone (like setting flow alone) is a necessary but not sufficient criterion for volume control, the control variable is
300:
Every breath is volume cycled, which is a form of machine cycling. Any breath for which inspiration is machine cycled is classified as a mandatory breath. Hence, the breath sequence is continuous mandatory
572:(PEEP) is pressure applied upon expiration. PEEP is applied using either a valve that is connected to the expiratory port and set manually or a valve managed internally by a mechanical ventilator.
222:
Adaptive: A targeting scheme that allows the ventilator to automatically set one target (eg, pressure within a breath) to achieve another target (eg, average tidal volume over several breaths).
185:
Breaths are classified by the criteria that trigger (start) and cycle (stop) inspiration. The start of inspiration is called the trigger event. The end of inspiration is called the cycle event.
579:
to remain open and not fully deflate. This mechanism for maintaining inflated alveoli helps increase partial pressure of oxygen in arterial blood, and an increase in PEEP increases the PaO
218:
Bio-variable: A targeting scheme that allows the ventilator to automatically set the inspiratory pressure or tidal volume randomly to mimic the variability observed during normal breathing.
180:
Time control (TC) means that, in some rare situations, none of the main variables (pressure, volume, or flow) are preset. In this case only the inspiratory and expiratory times are preset.
453:
open and not fully deflate. This mechanism for maintaining inflated alveoli helps increase partial pressure of oxygen in arterial blood, an appropriate increase in CPAP increases the PaO
703:
The ventilator varies the tidal volume and pressure based on the patient's work of breathing. The amount it delivers is proportional to the percentage of assistance it is set to give.
1983:
Chatburn, Robert L., Mireles-Cabodevila E., "Closed-loop control of mechanical ventilation: description and classification of targeting schemes", Respiratory Care, 56(1), 85-102, 2011.
390:
Intermittent mandatory ventilation has not always had the synchronized feature, so the division of modes were understood to be SIMV (synchronized) vs IMV (not-synchronized). Since the
1680:
595:(PSV). The patient initiates every breath and the ventilator delivers support with the preset pressure value. With support from the ventilator, the patient also regulates their own
214:
Set-point: A targeting scheme for which the operator sets all the parameters of the pressure waveform (pressure control modes) or volume and flow waveforms (volume control modes).
2001:
Tehrani, Fleur T., Automatic control of mechanical ventilation. Part 2: the existing techniques and future trends, Journal of Clinical Monitoring and Computing 22 (2008) 417–424.
278:
Step 2: Identify the breath sequence. Determine whether trigger and cycle events are patient or machine determined. Then, use this information to determine the breath sequence.
2285:
1992:
Tehrani, Fleur T., Automatic control of mechanical ventilation. Part 1: theory and history of the technology, Journal of Clinical Monitoring and Computing 22 (2008) 409–415.
369:
is a time-cycled alternant between two levels of positive airway pressure, with the main time on the high level and a brief expiratory release to facilitate ventilation.
1182:
2295:
324:
The ventilator adjusts inspiratory pressure between breaths to achieve an average preset tidal volume, so the targeting scheme is adaptive. The mode tag is PC-IMVa,s.
1710:
Barnes T, Enk D. Ventilation for low dissipated energy achieved using flow control during both inspiration and expiration. Trends Anaesth Crit Care. 2019;24:5–12.
2331:
422:
MMV is an optimal mode for weaning in neonatal and pediatric populations and has been shown to reduce long-term complications related to mechanical ventilation.
696:
Proportional assist ventilation (PAV) is another servo targeting based mode in which the ventilator guarantees the percentage of work regardless of changes in
434:
The peak inspiratory pressure delivered by the ventilator is varied on a breath-to-breath basis to achieve a target tidal volume that is set by the clinician.
2336:
685:
Neurally Adjusted Ventilatory Assist (NAVA) is adjusted by a computer (servo) and is similar to ATC but with more complex requirements for implementation.
2346:
1239:
1231:
1112:
991:
688:
In terms of patient-ventilator synchrony, NAVA supports both resistive and elastic work of breathing in proportion to the patient's inspiratory effort
674:
Automatic Tube Compensation (ATC) is the simplest example of a computer-controlled targeting system on a ventilator. It is a form of servo targeting.
1051:
1047:
1681:
https://depatisnet.dpma.de/DepatisNet/depatisnet?window=1&space=menu&content=treffer&action=pdf&docid=DE102016109528A1&xxxfull=1
2230:
1561:
1420:"Non-invasive ventilation for the management of acute hypercapnic respiratory failure due to exacerbation of chronic obstructive pulmonary disease"
1364:
1293:
1243:
1217:
1173:
1139:
42:
1523:
1165:
1569:
1378:
1572:(October 1982). "Comparison of high frequency jet ventilation to conventional ventilation during severe acute respiratory failure in humans".
1524:"High-frequency oscillatory ventilation in adult patients with acute respiratory distress syndrome: Where do we stand and where should we go?"
89:
1324:
1153:
1099:
61:
1328:
1316:
1306:
Benzer H (1988) Ventilatory support by intermittent changes in PEEP levels. 4th European Congress on Intensive Care Medicine. Baveno-Stresa
1332:
1169:
1161:
1103:
1095:
2046:
Degraeuwe PL, Vos GD, Blanco CE (1995). "Perfluorochemical liquid ventilation: from the animal laboratory to the intensive care unit".
1691:
Enk D: Gasstromumkehrelement (gas flow reversing element). Patent application (DE 10 2007 013 385 A1). German Patent Office, 16.03.2007
1565:
739:
Despite its theoretical advantages, efficacy studies have been disappointing and the optimal clinical use of LV has yet to be defined.
68:
465:
216:
Dual: A targeting scheme that allows the ventilator to switch between volume control and pressure control during a single inspiration.
1320:
1177:
1157:
1107:
1091:
391:
265:
intelligent = i. A tag is an abbreviation for a mode classification, such as PC-IMVs,s. Compound tags are possible, eg, PC-IMVoi,oi.
782:
1679:
Enk D. Verfahren und Vorrichtung zur Beatmung eines Patienten (method and device for ventilating a patient). (2017) Available at:
513:
BPAP has been shown to be useful in reducing mortality and reducing the need for endotracheal intubation when used in people with
75:
2263:
395:
134:
1865:
1252:"A crossover analysis of mandatory minute ventilation compared to synchronized intermittent mandatory ventilation in neonates"
2258:
514:
487:
57:
2223:
706:
PAV, like NAVA, supports both restrictive and elastic work of breathing in proportion to the patient's inspiratory effort.
1912:
449:(CPAP) is a non-invasive positive pressure mode of respiratory support. CPAP is a continuous pressure applied to keep the
156:
flow to the start of inspiratory flow. The flow-time curve is the basis for many variables related to ventilator settings.
2362:
2321:
2316:
1933:
Tehrani FT. Method and apparatus for controlling an artificial respiratory. US patent 4,986,268, issued January 22, 1991.
1337:
1180:(July 2001). "Long-term effects of spontaneous breathing during ventilatory support in patients with acute lung injury".
446:
366:
2300:
2281:
1419:
1152:
372:
Airway pressure release ventilation is usually utilized as a type of inverse ratio ventilation. The exhalation time (T
1621:
MAQUET, "Modes of ventilation in SERVO-s, invasive and non-invasive", 2009 MAQUET Critical Care AB, Order No 66 61 131
1230:
2402:
1960:
1383:
108:
2598:
2418:
2290:
569:
476:
2603:
2392:
2216:
486:
CPAP/APAP, BPAP, and other non-invasive ventilation modes have been shown to be effective management tools for
46:
1110:(September 1989). "[Biphasic positive airway pressure (BIPAP)--a new form of augmented ventilation]".
1910:
Walkey, Allan M.D. and Ross Summer M.D., "Negative pressure" in "E. Noninvasive Mechanical Ventilation," in
1891:
648:
Various "negative pressure ventilators" (NPVs) have been developed to serve this function—most famously the "
501:
Often BPAP is incorrectly referred to as "BiPAP". BiPAP is the name of a portable ventilator manufactured by
82:
1898:, retrieved April 11, 2020 (historical background and images, explanatory diagrams, and live demonstrations)
2593:
2450:
2326:
637:
732:
Providing a reservoir in which oxygen and carbon dioxide can be exchanged with pulmonary capillary blood
2567:
2341:
1381:(November 2001). "A prospective, randomized trial of BiPAP in severe acute congestive heart failure".
281:
Step 3: Identify the targeting schemes for the primary breaths and (if applicable) secondary breaths.
2442:
491:
236:
2479:
2310:
2305:
2011:
Younes M (1992). "Proportional assist ventilation, a new approach to ventilatory support. Theory".
1847:
480:
379:
Different perceptions of this mode may exist around the globe. While 'APRV' is common to users in
1870:
1838:
1609:
1256:
1000:
502:
35:
2089:
Norris MK, Fuhrman BP, Leach CL (1994). "Liquid ventilation: it's not science fiction anymore".
2239:
1634:
1574:
1335:(January 1994). "Biphasic positive airway pressure (BIPAP)—a new mode of ventilatory support".
787:
717:
is a technique of mechanical ventilation in which the lungs are insufflated with an oxygenated
220:
Servo: A targeting scheme for which inspiratory pressure is proportional to inspiratory effort.
128:. The mode refers to the method of inspiratory support. In general, mode selection is based on
125:
2538:
1815:
1418:
Osadnik, CR; Tee, VS; Carson-Chahhoud, KV; Picot, J; Wedzicha, JA; Smith, BJ (13 July 2017).
1358:
1287:
1211:
1133:
1056:
798:
129:
1315:
677:
The goal of ATC is to support the resistive work of breathing through the artificial airway
358:
2608:
2458:
2382:
2377:
1054:(July 2011). "Airway pressure release ventilation in acute respiratory distress syndrome".
902:
697:
530:
and piston force positive pressure in and apply negative pressure to force an expiration.
8:
1841:
School of Medicine & Public Health, William S. Middleton Memorial Veterans Hospital,
1554:
1090:
321:
Spontaneous breaths are allowed between mandatory breaths so the breath sequence is IMV.
146:
The taxonomy is a logical classification system based on 10 maxims of ventilator design
2522:
2495:
2186:
Cox CA, Wolfson MR, Shaffer TH (1996). "Liquid ventilation: a comprehensive overview".
2071:
1966:
1842:
1811:
1659:
1504:
1455:
1024:
995:
932:
714:
576:
450:
1396:
2562:
2530:
2195:
2168:
2133:
2106:
2063:
2028:
1956:
1919:
1651:
1591:
1587:
1543:
1496:
1460:
1400:
1346:
1275:
1199:
1121:
1073:
1029:
973:
924:
883:
842:
793:
718:
438:(PC) settings fundamentally PRVC is a pressure-control mode with adaptive targeting.
2075:
1970:
1663:
1508:
936:
610:
Pressure support improves oxygenation, ventilation and decreases work of breathing.
2572:
2503:
2466:
2160:
2124:
Greenspan JS (1996). "Physiology and clinical role of liquid ventilation therapy".
2098:
2055:
2020:
1948:
1820:
1643:
1583:
1535:
1488:
1450:
1442:
1438:
1434:
1392:
1265:
1247:
1191:
1065:
1019:
1009:
963:
916:
873:
834:
596:
227:
Intelligent: A targeting scheme that uses artificial intelligence programs such as
1608:
MAQUET, "Modes of ventilation in SERVO-i, invasive and non-invasive", 2008 MAQUET
729:
Opening of collapsed alveoli by hydraulic pressure with a lower risk of barotrauma
2397:
1647:
1539:
1492:
1195:
838:
774:
398:
the "synchronized" part of the title has been dropped and now there is only IMV.
1806:
1804:
333:
Mechanical ventilation machines are available with both invasive modes (such as
2367:
2151:
Dirkes S (1996). "Liquid ventilation: new frontiers in the treatment of ARDS".
2102:
2059:
2024:
1882:
1880:
1952:
1887:
1069:
2587:
1801:
380:
232:
2164:
1877:
164:
fact is known as the equation of motion for the passive respiratory system:
2487:
1833:
1831:
1655:
1560:
1547:
1500:
1464:
1446:
1404:
1279:
1203:
1077:
1033:
977:
968:
951:
928:
920:
887:
846:
600:
338:
2199:
2172:
2137:
2110:
2067:
2032:
1595:
1350:
1270:
1251:
1125:
297:
Inspiratory volume and flow are preset, so the control variable is volume.
2208:
1816:"Non-invasive and domiciliary ventilation: negative pressure techniques,"
907:
804:
495:
228:
1828:
2387:
1860:
1858:
1235:
878:
861:
575:
PEEP is a pressure that an exhalation has to bypass, in effect causing
553:
334:
790: – Method to mechanically assist or replace spontaneous breathing
726:
Reducing surface tension by maintaining a fluid interface with alveoli
2372:
1046:
649:
645:
voluntary (or involuntary) inhalation through the patient's airway.
344:
1943:
Tehrani FT (1991). "Automatic control of an artificial respirator".
1855:
24:
1014:
949:
607:
regulate the pressure support level to obtain desired ventilation.
310:
290:
2434:
1906:
1904:
1895:
1479:
noninvasive ventilation in pediatric acute respiratory failure".
591:
Pressure support is a spontaneous mode of ventilation also named
903:"Determining the Basis for a Taxonomy of Mechanical Ventilation"
1901:
1417:
952:"A taxonomy for mechanical ventilation: 10 fundamental maxims"
2550:
901:
Chatburn RL, Volsko TA, Hazy J, Harris LN, Sanders S (2011).
559:
284:
275:
is volume. If neither is true, the control variable is time.
250:
Control Variable (Pressure or Volume, for the primary breath)
505:; it is just one of many ventilators that can deliver BPAP.
2426:
1890:, video (8 minutes), January 11, 2016, OPENPediatrics and
1477:
1183:
American Journal of Respiratory and Critical Care Medicine
616:
900:
950:
Chatburn RL, El-Khatib M, Mireles-Cabodevila E (2014).
823:
680:
533:
520:
441:
353:
141:
124:
are one of the most important aspects of the usage of
1810:
Shneerson, Dr. John M., Newmarket General Hospital, (
1675:
1673:
1630:
748:
oxygenate and remove carbon dioxide from the liquid.
460:
167:
Pressure = (Elastance × Volume) + (Resistance × Flow)
807: – Noninvasive form of ventilation for newborns
764:
425:
564:
471:
49:. Unsourced material may be challenged and removed.
2088:
2045:
1864:Grum, Cyril M., MD, and Melvin L. Morganroth, MD,
1670:
1521:
691:
345:Assist mode, control mode, and assist-control mode
2185:
801: – Practitioner in cardio-pulmonary medicine
2585:
990:
630:
256:Primary Breath Targeting Scheme (for CMV or CSV)
735:Functioning as a high-efficiency heat exchanger
660:
401:
328:
669:
621:
2224:
1825:1991;46: pp.131-135, retrieved April 12, 2020
751:
2123:
1624:
1515:
1377:
1363:: CS1 maint: multiple names: authors list (
1292:: CS1 maint: multiple names: authors list (
1216:: CS1 maint: multiple names: authors list (
1138:: CS1 maint: multiple names: authors list (
2179:
2144:
2117:
2082:
2039:
1427:The Cochrane Database of Systematic Reviews
894:
862:"Neonatal ventilators: how do they differ?"
853:
742:
269:
259:Secondary Breath Targeting Scheme (for IMV)
2238:
2231:
2217:
638:Main article: Negative pressure ventilator
560:Spontaneous breathing and support settings
285:Example mode classification is given below
1454:
1269:
1023:
1013:
967:
877:
411:x f, no mandatory breaths are delivered.
392:American Association for Respiratory Care
362:Airway pressure release ventilation graph
109:Learn how and when to remove this message
2150:
783:Table of modes of mechanical ventilation
357:
1942:
1818:#5 of series "Assisted ventilation" in
859:
613:Also see adaptive support ventilation.
2586:
2264:Nomenclature of mechanical ventilation
2010:
655:
617:Other ventilation modes and strategies
396:nomenclature of mechanical ventilation
135:nomenclature of mechanical ventilation
2259:Mechanical ventilation in emergencies
2212:
1913:Boston Medical Center ICU Manual 2008
1874:1988;3:6-20, retrieved April 12, 2020
709:
515:chronic obstructive pulmonary disease
488:chronic obstructive pulmonary disease
309:Mode Name: SIMV Volume Control Plus (
133:have been substantial changes in the
1866:"Initiating Mechanical Ventilation,"
681:Neurally Adjusted Ventilatory Assist
534:High-frequency ventilation (Passive)
47:adding citations to reliable sources
18:
1338:European Journal of Anaesthesiology
586:
546:
521:High-frequency ventilation (Active)
447:Continuous positive airway pressure
442:Continuous positive airway pressure
367:Airway pressure release ventilation
354:Airway pressure release ventilation
142:Taxonomy for mechanical ventilation
13:
466:Automatic positive airway pressure
461:Automatic positive airway pressure
337:) and non-invasive modes (such as
253:Breath Sequence (CMV, IMV, or CSV)
14:
2620:
2403:Ventilator-associated lung injury
1947:. Vol. 13. pp. 1738–9.
1384:The Journal of Emergency Medicine
426:Pressure-regulated volume control
58:"Modes of mechanical ventilation"
1588:10.1097/00003246-198210000-00001
1481:Pediatric Critical Care Medicine
767:
570:Positive end expiratory pressure
565:Positive end-expiratory pressure
477:Bilevel positive airway pressure
472:Bilevel positive airway pressure
23:
2393:Ventilator-associated pneumonia
2254:Modes of mechanical ventilation
2091:AACN Clin Issues Crit Care Nurs
2004:
1995:
1986:
1977:
1936:
1927:
1924:p.17, retrieved April 12, 2020.
1791:
1781:
1772:
1763:
1753:
1743:
1733:
1723:
1713:
1704:
1694:
1685:
1615:
1602:
1471:
1411:
1371:
1309:
1300:
692:Proportional Assist Ventilation
508:
289:Mode Name: A/C Volume Control (
122:Modes of mechanical ventilation
34:needs additional citations for
1439:10.1002/14651858.CD004104.pub4
1224:
1146:
1084:
1040:
984:
943:
817:
16:Methods of inspiratory support
1:
1750:10.1097/CCM.0000000000004209.
1730:10.1097/EJA.0000000000001326.
1397:10.1016/s0736-4679(01)00385-7
811:
631:Negative pressure ventilation
479:(BPAP) is a mode used during
1648:10.1097/CCM.0b013e318206bda6
1540:10.1097/CCM.0b013e31822a5c35
1493:10.1097/PCC.0b013e318184989f
1196:10.1164/ajrccm.164.1.2001078
839:10.1164/ajrccm.161.5.9902018
661:Adaptive Support Ventilation
593:Pressure Support Ventilation
402:Mandatory minute ventilation
329:Descriptions of common modes
149:
7:
1760:10.1186/s13054-020-03325-3.
1522:Allardet-Servent J (2011).
1008:(1). London, England: 115.
760:
670:Automatic Tube Compensation
622:Flow-controlled ventilation
552:volume control to minimize
10:
2625:
2103:10.4037/15597768-1994-3004
2060:10.1177/039139889501801020
1892:Boston Children's Hospital
1888:"The Iron Lung and Polio,"
752:Partial liquid ventilation
237:artificial neural networks
2515:
2478:
2411:
2355:
2347:List of modes by category
2272:
2246:
1953:10.1109/IEMBS.1991.684729
1837:Matioc, Adrian A., M.D.,
1070:10.1016/j.ccc.2011.05.003
827:Am J Respir Crit Care Med
492:acute respiratory failure
2025:10.1164/ajrccm/145.1.114
1812:Newmarket, Suffolk, U.K.
996:"What on earth is APRV?"
743:Total liquid ventilation
481:non-invasive ventilation
270:How modes are classified
2599:Intensive care medicine
2165:10.4037/ccn1996.16.3.53
1871:Intensive Care Medicine
1839:University of Wisconsin
1257:Journal of Perinatology
503:Respironics Corporation
2604:Mechanical ventilation
2240:Mechanical ventilation
1635:Critical Care Medicine
1612:AB, Order No 66 14 692
1575:Critical Care Medicine
969:10.4187/respcare.03057
921:10.4187/respcare.01327
788:Mechanical ventilation
363:
267:
241:
195:
182:
169:
126:mechanical ventilation
2132:(2 Pt 2 Su): S47-52.
1886:Rockoff, Mark, M.D.,
1740:EJA.0000000000000819.
1271:10.1038/sj.jp.7211371
1057:Critical Care Clinics
799:Respiratory therapist
361:
262:
212:
190:
172:
165:
2383:Pulmonary volutrauma
2378:Pulmonary barotrauma
698:pulmonary compliance
43:improve this article
2594:Respiratory therapy
1945:Proc IEEE EMBS Conf
656:Closed loop systems
2048:Int J Artif Organs
1843:Madison, Wisconsin
1720:10.1111/aas.13526.
879:10.1038/jp.2009.23
872:(Suppl 2): S73-8.
715:Liquid ventilation
710:Liquid ventilation
364:
2581:
2580:
2013:Am Rev Respir Dis
1920:Boston University
1240:Bonnie J. Lafleur
794:Prone ventilation
719:perfluorochemical
119:
118:
111:
93:
2616:
2573:Mechanical power
2233:
2226:
2219:
2210:
2209:
2204:
2203:
2183:
2177:
2176:
2148:
2142:
2141:
2121:
2115:
2114:
2086:
2080:
2079:
2043:
2037:
2036:
2008:
2002:
1999:
1993:
1990:
1984:
1981:
1975:
1974:
1940:
1934:
1931:
1925:
1908:
1899:
1884:
1875:
1862:
1853:
1835:
1826:
1808:
1799:
1795:
1789:
1785:
1779:
1776:
1770:
1767:
1761:
1757:
1751:
1747:
1741:
1737:
1731:
1727:
1721:
1717:
1711:
1708:
1702:
1698:
1692:
1689:
1683:
1677:
1668:
1667:
1628:
1622:
1619:
1613:
1606:
1600:
1599:
1558:
1552:
1551:
1519:
1513:
1512:
1475:
1469:
1468:
1458:
1424:
1415:
1409:
1408:
1375:
1369:
1368:
1362:
1354:
1313:
1307:
1304:
1298:
1297:
1291:
1283:
1273:
1250:(October 2005).
1248:William F. Walsh
1232:Scott O. Guthrie
1228:
1222:
1221:
1215:
1207:
1150:
1144:
1143:
1137:
1129:
1113:Der Anaesthesist
1088:
1082:
1081:
1044:
1038:
1037:
1027:
1017:
992:Dietrich Henzler
988:
982:
981:
971:
947:
941:
940:
898:
892:
891:
881:
860:Donn SM (2009).
857:
851:
850:
821:
777:
772:
771:
770:
700:and resistance.
597:respiratory rate
587:Pressure support
547:Volume guarantee
114:
107:
103:
100:
94:
92:
51:
27:
19:
2624:
2623:
2619:
2618:
2617:
2615:
2614:
2613:
2584:
2583:
2582:
2577:
2558:
2554:
2546:
2542:
2534:
2526:
2511:
2507:
2499:
2491:
2474:
2470:
2462:
2454:
2446:
2438:
2430:
2422:
2407:
2398:Oxygen toxicity
2356:Related illness
2351:
2268:
2242:
2237:
2207:
2184:
2180:
2153:Crit Care Nurse
2149:
2145:
2122:
2118:
2087:
2083:
2044:
2040:
2009:
2005:
2000:
1996:
1991:
1987:
1982:
1978:
1963:
1941:
1937:
1932:
1928:
1909:
1902:
1885:
1878:
1863:
1856:
1852:Vol. 128, No 2.
1836:
1829:
1809:
1802:
1796:
1792:
1786:
1782:
1777:
1773:
1768:
1764:
1758:
1754:
1748:
1744:
1738:
1734:
1728:
1724:
1718:
1714:
1709:
1705:
1699:
1695:
1690:
1686:
1678:
1671:
1629:
1625:
1620:
1616:
1607:
1603:
1582:(10): 625–630.
1559:
1555:
1520:
1516:
1476:
1472:
1433:(7): CD004104.
1422:
1416:
1412:
1376:
1372:
1356:
1355:
1314:
1310:
1305:
1301:
1285:
1284:
1264:(10): 643–646.
1229:
1225:
1209:
1208:
1151:
1147:
1131:
1130:
1089:
1085:
1052:Lewis J. Kaplan
1048:Adrian A. Maung
1045:
1041:
989:
985:
962:(11): 1747–63.
948:
944:
899:
895:
858:
854:
822:
818:
814:
775:Medicine portal
773:
768:
766:
763:
754:
745:
712:
694:
683:
672:
663:
658:
633:
624:
619:
589:
582:
567:
562:
549:
536:
523:
511:
474:
463:
456:
444:
428:
418:
410:
404:
375:
356:
347:
331:
287:
272:
226:
223:
221:
219:
217:
215:
179:
176:
152:
144:
115:
104:
98:
95:
52:
50:
40:
28:
17:
12:
11:
5:
2622:
2612:
2611:
2606:
2601:
2596:
2579:
2578:
2576:
2575:
2570:
2565:
2560:
2556:
2552:
2548:
2544:
2540:
2536:
2532:
2528:
2524:
2519:
2517:
2513:
2512:
2510:
2509:
2505:
2501:
2497:
2493:
2489:
2484:
2482:
2476:
2475:
2473:
2472:
2468:
2464:
2460:
2456:
2452:
2448:
2444:
2440:
2436:
2432:
2428:
2424:
2420:
2415:
2413:
2409:
2408:
2406:
2405:
2400:
2395:
2390:
2385:
2380:
2375:
2370:
2368:Atelectotrauma
2365:
2359:
2357:
2353:
2352:
2350:
2349:
2344:
2339:
2334:
2329:
2324:
2319:
2314:
2308:
2303:
2298:
2293:
2288:
2278:
2276:
2270:
2269:
2267:
2266:
2261:
2256:
2250:
2248:
2244:
2243:
2236:
2235:
2228:
2221:
2213:
2206:
2205:
2178:
2143:
2116:
2081:
2054:(10): 674–83.
2038:
2019:(1): 114–120.
2003:
1994:
1985:
1976:
1961:
1935:
1926:
1900:
1876:
1854:
1848:Anesthesiology
1827:
1800:
1790:
1780:
1771:
1762:
1752:
1742:
1732:
1722:
1712:
1703:
1693:
1684:
1669:
1623:
1614:
1601:
1562:D. P. Schuster
1553:
1534:(12): 2761–2.
1514:
1470:
1410:
1370:
1308:
1299:
1244:Steven M. Donn
1223:
1174:T. Von Spiegel
1145:
1120:(9): 452–458.
1083:
1064:(3): 501–509.
1039:
1015:10.1186/cc9419
983:
942:
893:
852:
815:
813:
810:
809:
808:
802:
796:
791:
785:
779:
778:
762:
759:
753:
750:
744:
741:
737:
736:
733:
730:
727:
711:
708:
693:
690:
682:
679:
671:
668:
662:
659:
657:
654:
642:
641:
632:
629:
623:
620:
618:
615:
588:
585:
580:
566:
563:
561:
558:
548:
545:
535:
532:
522:
519:
510:
507:
473:
470:
462:
459:
454:
443:
440:
427:
424:
416:
408:
403:
400:
394:established a
373:
355:
352:
346:
343:
330:
327:
326:
325:
322:
319:
307:
306:
302:
298:
286:
283:
271:
268:
261:
260:
257:
254:
251:
247:
246:
242:
233:expert systems
208:
204:
200:
196:
186:
183:
161:
157:
151:
148:
143:
140:
117:
116:
31:
29:
22:
15:
9:
6:
4:
3:
2:
2621:
2610:
2607:
2605:
2602:
2600:
2597:
2595:
2592:
2591:
2589:
2574:
2571:
2569:
2566:
2564:
2561:
2559:
2549:
2547:
2537:
2535:
2529:
2527:
2521:
2520:
2518:
2514:
2508:
2502:
2500:
2494:
2492:
2486:
2485:
2483:
2481:
2477:
2471:
2465:
2463:
2457:
2455:
2449:
2447:
2441:
2439:
2433:
2431:
2425:
2423:
2417:
2416:
2414:
2410:
2404:
2401:
2399:
2396:
2394:
2391:
2389:
2386:
2384:
2381:
2379:
2376:
2374:
2371:
2369:
2366:
2364:
2361:
2360:
2358:
2354:
2348:
2345:
2343:
2340:
2338:
2335:
2333:
2330:
2328:
2325:
2323:
2320:
2318:
2315:
2312:
2309:
2307:
2304:
2302:
2299:
2297:
2294:
2292:
2289:
2287:
2283:
2280:
2279:
2277:
2275:
2271:
2265:
2262:
2260:
2257:
2255:
2252:
2251:
2249:
2245:
2241:
2234:
2229:
2227:
2222:
2220:
2215:
2214:
2211:
2201:
2197:
2193:
2189:
2188:Neonatal Netw
2182:
2174:
2170:
2166:
2162:
2158:
2154:
2147:
2139:
2135:
2131:
2127:
2120:
2112:
2108:
2104:
2100:
2097:(3): 246–54.
2096:
2092:
2085:
2077:
2073:
2069:
2065:
2061:
2057:
2053:
2049:
2042:
2034:
2030:
2026:
2022:
2018:
2014:
2007:
1998:
1989:
1980:
1972:
1968:
1964:
1962:0-7803-0216-8
1958:
1954:
1950:
1946:
1939:
1930:
1923:
1921:
1916:
1914:
1907:
1905:
1897:
1893:
1889:
1883:
1881:
1873:
1872:
1867:
1861:
1859:
1851:
1849:
1844:
1840:
1834:
1832:
1824:
1822:
1817:
1813:
1807:
1805:
1794:
1784:
1775:
1766:
1756:
1746:
1736:
1726:
1716:
1707:
1697:
1688:
1682:
1676:
1674:
1665:
1661:
1657:
1653:
1649:
1645:
1642:(4): 746–55.
1641:
1637:
1636:
1627:
1618:
1611:
1610:Critical Care
1605:
1597:
1593:
1589:
1585:
1581:
1577:
1576:
1571:
1567:
1563:
1557:
1549:
1545:
1541:
1537:
1533:
1529:
1528:Crit Care Med
1525:
1518:
1510:
1506:
1502:
1498:
1494:
1490:
1486:
1482:
1474:
1466:
1462:
1457:
1452:
1448:
1447:10044/1/53458
1444:
1440:
1436:
1432:
1428:
1421:
1414:
1406:
1402:
1398:
1394:
1390:
1386:
1385:
1380:
1374:
1366:
1360:
1352:
1348:
1344:
1340:
1339:
1334:
1330:
1326:
1322:
1318:
1312:
1303:
1295:
1289:
1281:
1277:
1272:
1267:
1263:
1259:
1258:
1253:
1249:
1245:
1241:
1237:
1233:
1227:
1219:
1213:
1205:
1201:
1197:
1193:
1189:
1185:
1184:
1179:
1175:
1171:
1167:
1166:J. Zinserling
1163:
1159:
1155:
1149:
1141:
1135:
1127:
1123:
1119:
1115:
1114:
1109:
1105:
1101:
1097:
1093:
1087:
1079:
1075:
1071:
1067:
1063:
1059:
1058:
1053:
1049:
1043:
1035:
1031:
1026:
1021:
1016:
1011:
1007:
1003:
1002:
1001:Critical Care
997:
993:
987:
979:
975:
970:
965:
961:
957:
953:
946:
938:
934:
930:
926:
922:
918:
915:(4): 514–24.
914:
910:
909:
904:
897:
889:
885:
880:
875:
871:
867:
863:
856:
848:
844:
840:
836:
833:(5): 1450–8.
832:
828:
820:
816:
806:
803:
800:
797:
795:
792:
789:
786:
784:
781:
780:
776:
765:
758:
749:
740:
734:
731:
728:
725:
724:
723:
720:
716:
707:
704:
701:
699:
689:
686:
678:
675:
667:
653:
651:
646:
640:
639:
635:
634:
628:
614:
611:
608:
604:
602:
598:
594:
584:
578:
573:
571:
557:
555:
544:
541:
531:
528:
518:
516:
506:
504:
499:
497:
493:
489:
484:
482:
478:
469:
467:
458:
452:
448:
439:
435:
432:
423:
420:
412:
399:
397:
393:
388:
384:
382:
381:North America
377:
370:
368:
360:
351:
342:
340:
336:
323:
320:
316:
315:
314:
312:
303:
299:
296:
295:
294:
292:
282:
279:
276:
266:
258:
255:
252:
249:
248:
243:
240:
238:
234:
231:, rule based
230:
209:
205:
201:
197:
194:
187:
184:
181:
168:
162:
158:
154:
153:
147:
139:
136:
131:
127:
123:
113:
110:
102:
91:
88:
84:
81:
77:
74:
70:
67:
63:
60: –
59:
55:
54:Find sources:
48:
44:
38:
37:
32:This article
30:
26:
21:
20:
2568:A-a gradient
2273:
2253:
2247:Fundamentals
2194:(3): 31–43.
2191:
2187:
2181:
2156:
2152:
2146:
2129:
2125:
2119:
2094:
2090:
2084:
2051:
2047:
2041:
2016:
2012:
2006:
1997:
1988:
1979:
1944:
1938:
1929:
1918:
1911:
1869:
1846:
1819:
1793:
1783:
1774:
1765:
1755:
1745:
1735:
1725:
1715:
1706:
1701:121:167–176.
1696:
1687:
1639:
1633:
1626:
1617:
1604:
1579:
1573:
1570:J. V. Snyder
1556:
1531:
1527:
1517:
1487:(5): 484–9.
1484:
1480:
1473:
1430:
1426:
1413:
1391:(4): 363–9.
1388:
1382:
1379:M. A. Levitt
1373:
1359:cite journal
1345:(1): 37–42.
1342:
1336:
1311:
1302:
1288:cite journal
1261:
1255:
1226:
1212:cite journal
1190:(1): 43–49.
1187:
1181:
1148:
1134:cite journal
1117:
1111:
1086:
1061:
1055:
1042:
1005:
999:
986:
959:
955:
945:
912:
906:
896:
869:
865:
855:
830:
826:
819:
755:
746:
738:
713:
705:
702:
695:
687:
684:
676:
673:
664:
647:
643:
636:
625:
612:
609:
605:
601:tidal volume
592:
590:
574:
568:
550:
539:
537:
526:
524:
512:
509:Medical uses
500:
485:
475:
464:
445:
436:
433:
429:
421:
413:
405:
389:
385:
378:
371:
365:
348:
332:
308:
301:ventilation.
288:
280:
277:
273:
263:
213:
191:
173:
166:
145:
121:
120:
105:
96:
86:
79:
72:
65:
53:
41:Please help
36:verification
33:
2609:Pulmonology
2159:(3): 53–8.
2126:J Perinatol
1325:C. Putensen
1154:C. Putensen
1100:C. Putensen
956:Respir Care
908:Respir Care
866:J Perinatol
805:Bubble CPAP
496:sleep apnea
229:fuzzy logic
178:resistance.
175:resistance.
2588:Categories
2388:Rheotrauma
1329:N. J. Mutz
1317:C. Hormann
1236:Chris Lynn
812:References
599:and their
554:volutrauma
335:intubation
313:PB 840):
305:(VC-CMVs).
293:PB 840):
99:April 2020
69:newspapers
2373:Biotrauma
1333:H. Benzer
1170:F. Stuber
1162:H. Wrigge
1104:W. Koller
1096:H. Benzer
650:Iron lung
538:The term
525:The term
318:pressure.
225:pattern).
150:10 maxims
130:clinician
2412:Pressure
2076:13038566
1971:63221714
1664:35876431
1656:21263322
1566:M. Klain
1548:22094505
1509:20821767
1501:18679148
1465:28702957
1405:11728761
1280:16079905
1204:11435237
1078:21742214
1034:21345265
994:(2011).
978:25118309
937:27417478
929:22004898
888:19399015
847:10806138
761:See also
517:(COPD).
311:Covidien
291:Covidien
2480:Volumes
2200:8715647
2173:8852261
2138:8732549
2111:7780839
2068:8647601
2033:1731573
1917:2008,
1896:YouTube
1788:(2022).
1596:6749433
1456:6483555
1351:8143712
1321:M. Baum
1178:N. Mutz
1158:S. Zech
1126:2686487
1108:G. Putz
1092:M. Baum
1025:3222047
577:alveoli
540:passive
498:, etc.
451:alveoli
245:levels:
83:scholar
2533:static
2198:
2171:
2136:
2109:
2074:
2066:
2031:
1969:
1959:
1821:Thorax
1798:(2022)
1662:
1654:
1594:
1568:&
1546:
1507:
1499:
1463:
1453:
1403:
1349:
1331:&
1278:
1246:&
1202:
1176:&
1124:
1106:&
1076:
1050:&
1032:
1022:
976:
935:
927:
886:
845:
527:active
235:, and
85:
78:
71:
64:
56:
2516:Other
2274:Modes
2072:S2CID
1967:S2CID
1660:S2CID
1505:S2CID
1423:(PDF)
933:S2CID
207:rare.
90:JSTOR
76:books
2469:plat
2363:ARDS
2322:APRV
2317:CPAP
2313:/NIV
2311:BPAP
2286:SIMV
2196:PMID
2169:PMID
2134:PMID
2107:PMID
2064:PMID
2029:PMID
1957:ISBN
1652:PMID
1592:PMID
1544:PMID
1497:PMID
1461:PMID
1431:2017
1401:PMID
1365:link
1347:PMID
1294:link
1276:PMID
1218:link
1200:PMID
1140:link
1122:PMID
1074:PMID
1030:PMID
974:PMID
925:PMID
884:PMID
843:PMID
339:BPAP
62:news
2525:dyn
2427:FiO
2421:EEP
2342:HFV
2337:ASV
2332:PAV
2327:MMV
2306:PAP
2301:CSV
2296:ACV
2291:CMV
2282:IMV
2161:doi
2099:doi
2056:doi
2021:doi
2017:145
1949:doi
1894:on
1868:in
1814:),
1644:doi
1584:doi
1536:doi
1489:doi
1451:PMC
1443:hdl
1435:doi
1393:doi
1266:doi
1192:doi
1188:164
1066:doi
1020:PMC
1010:doi
964:doi
917:doi
874:doi
835:doi
831:161
374:low
45:by
2590::
2563:OI
2555:/V
2461:AW
2445:IP
2192:15
2190:.
2167:.
2157:16
2155:.
2130:16
2128:.
2105:.
2093:.
2070:.
2062:.
2052:18
2050:.
2027:.
2015:.
1965:.
1955:.
1903:^
1879:^
1857:^
1830:^
1803:^
1672:^
1658:.
1650:.
1640:39
1638:.
1590:.
1580:10
1578:.
1564:,
1542:.
1532:39
1530:.
1526:.
1503:.
1495:.
1483:.
1459:.
1449:.
1441:.
1429:.
1425:.
1399:.
1389:21
1387:.
1361:}}
1357:{{
1343:11
1341:.
1327:,
1323:,
1319:,
1290:}}
1286:{{
1274:.
1262:25
1260:.
1254:.
1242:,
1238:,
1234:,
1214:}}
1210:{{
1198:.
1186:.
1172:,
1168:,
1164:,
1160:,
1156:,
1136:}}
1132:{{
1118:38
1116:.
1102:,
1098:,
1094:,
1072:.
1062:27
1060:.
1028:.
1018:.
1006:15
1004:.
998:.
972:.
960:59
958:.
954:.
931:.
923:.
913:57
911:.
905:.
882:.
870:29
868:.
864:.
841:.
829:.
603:.
583:.
556:.
494:,
490:,
457:.
415:(V
2557:T
2553:D
2551:V
2545:2
2543:O
2541:A
2539:P
2531:C
2523:C
2506:f
2504:V
2498:E
2496:V
2490:T
2488:V
2467:P
2459:P
2453:S
2451:P
2443:P
2437:P
2435:Δ
2429:2
2419:P
2284:/
2232:e
2225:t
2218:v
2202:.
2175:.
2163::
2140:.
2113:.
2101::
2095:5
2078:.
2058::
2035:.
2023::
1973:.
1951::
1922:,
1915:,
1850:,
1823:,
1666:.
1646::
1598:.
1586::
1550:.
1538::
1511:.
1491::
1485:9
1467:.
1445::
1437::
1407:.
1395::
1367:)
1353:.
1296:)
1282:.
1268::
1220:)
1206:.
1194::
1142:)
1128:.
1080:.
1068::
1036:.
1012::
980:.
966::
939:.
919::
890:.
876::
849:.
837::
581:2
455:2
417:E
409:T
407:V
239:.
112:)
106:(
101:)
97:(
87:·
80:·
73:·
66:·
39:.
Text is available under the Creative Commons Attribution-ShareAlike License. Additional terms may apply.